Specimen GC12334
Maxilla, anterior segment of the coronal section of the head, injected, showing ulceration of the face resulting from a carcinoma of the air-sinus of the left. … Microscopically, re-examination confirms the presence of a tumour growth which is diffusely cellular and which might be a spheroidal-cell carcinoma or sarcoma.
(Specimen also listed as Bci6M38 – in the Charles Bell Collection, 1824)
“A section of the head of a patient who died in the Middlesex Hospital; when he first presented himself he had a large fungous Tumour which projected from the left side of his face, occupying the left side of the mouth, destroying the left side of his nose, and hiding the left eye. After some time, this Tumour burst, and ulcerated, and frequently bled, exhibiting all the features of Fungus Haematodes. The Tumour is seen to extend backwards and into the throat of the posterior nostrils.”

There is no date to indicate when the patient died. The patient’s head is part of the Charles Bell collection, and Charles Bell moved from Edinburgh to London in 1804; his Collection of anatomical and pathological specimens was bought by the Royal College of Surgeons Edinburgh, the removal of the specimens being overseen by Robert Knox in 1825. (Of course there is always the possibility that patient had died before Bell arrived in London, and that Bell purchased the head subsequently for his Collection.)
The ‘section’ of the man’s head is in a large cylindrical glass jar filled with preservative. Not only do we see how the Tumour has disfigured his face, but we may also – because his skull has been removed from the back – look inside his nasal and oral cavities, to observe how the Tumour has invaded the soft tissues. But if we are to remind ourselves that this was a person, not a pathological specimen, we should look instead at his face. The man has ginger stubble on his chin, and his hair is pale ginger too (although this may be an artefact of the preservative). His right eye is closed so that his expression – despite the terrible deformation of his features – appears peaceful.
We can ask many questions, all now unanswerable. He must have been born in the last years of the 18th century. What sort of a man was he and where did he live? What was his general physical and mental health like before the Tumour grew? How old was he when it first appeared? Did he ‘present’ himself at the hospital or did friends or relatives take him there? Where else could he have gone if the hospital had rejected him as an ‘incurable’? Was he relieved to be taken in by the hospital, or terrified lest his ultimate resting place would be in an anatomy museum? Did he assume he would die in hospital? How was he cared for? (There was no palliative care).
After the first shock of seeing a man’s head preserved in a jar – and shock at the idea of a man’s head being preserved in a jar – the overwhelming feeling is of sadness and sympathy; and sorrow that he was born long before medical care and surgery could have helped him.
From: Essays on the anatomy of expression in painting: Charles Bell, 1806; Longman, London.
Relaxation of languor, faintness, and sorrow.
The muscle which depresses the angles of the mouth is often accompanied in its action by that of the corrugator muscle which knits the eyebrows, and this again is combined frequently with the action of the central fibres of the frontal muscle.
The depressing of the angle of the mouth gives an air of despondence and languor to the countenance when accompanied with a general relaxation of the features, or, in other words, of the muscles. When the corrugator which knits the brows co-operates with it, there is mingled in the expression something of mental energy of moroseness or pain.
In sorrow, that general languor which we have now described pervades the whole countenance. The violence and tension of grief, the agitations, the restlessness, the lamentations, and the tumult, have, like all strong excitements, gradually exhausted the frame. Sadness and regret, with depression of spirits and fond recollections, have succeeded; and lassitude of the whole body, with dejection of face and heaviness of the eyes, are the most striking characteristics. The lips are relaxed and the lower jaw drops ; the upper eyelid falls down and half covers the pupil of the eye. The eye is frequently filled with tears, and the eyebrows take an inclination similar to that which the depression of the angles of the lips give to the mouth.
***
“WHY DO I CALL HIM GEORGE?” Joyce Gunn Cairns’ story
“I have a photograph of a family friend, George, as a young boy. He died in 1980, aged 61. George was born in 1918, with a hair lip and cleft palate, and the surgical procedure then was to provide him with a palate, and involved the removal of his top teeth and giving him a false plate. George came into my life when I was five or six years old, a year or two after my father died at the age of thirty-six. We lived at that time in the small mining village of Rosewell in Midlothian, and George was the village joiner. My mother and George became strong and lasting supports for each other, and my mother was grateful for his kindness towards us as children: always her first priority. She was glad of George’s steadiness of nature, and his offer to take us all out for a run in his car – still something of a novelty in the late 1950s. George continued to be a part of our life from then until he died, twenty-five years later.
Although I remember as a child noting something different about his appearance and speech, this awareness soon slipped away, and he became just George our friend, the man who brought us sweets and took us for picnics in his shiny car, fixing whatever needed fixed in the house. He never lived with us, but remained ‘part of the furniture’ when we moved to Bonnyrigg, only two miles distant. He lived in an old miner’s cottage in Rosewell, now gone and replaced: its interior remains in memory – coal fire, wee back kitchen, grandmother’s clock, outside coal sheds, horsehair chairs, all part of George’s solid, traditional and reliable ambience!
I can only remember one time throughout the years George was part of our life when I was reminded of his disability: I was in a shop with him and my mum, and when the woman behind the counter could not understand what he was saying and became irate, my mother gave this woman a lashing with her tongue. She, my mother, was very protective of George in this way.
When Andrew [Connell, Collections Manager] first showed me ‘George’ I felt a sense of shock on seeing his disfigurement. I was eager to draw him, but also felt apprehensive. However the more frequently I drew him, the less I seemed to notice his disfigurement; or if I did, it was never again with that same initial shock or recoil.

From the drawing you will see that there is nothing of the grotesque in my preconception of him. And so I called him ‘George’ in memory of my friend George.
There is something strangely moving about the way that love penetrates the surface appearance, just as it did for me with our dear friend.”
Joyce Gunn Cairns 2010
***
Specimen GC8184 
Portion of a child, showing congenital malformation of the Nose.
From a female aged 3 weeks, who died of asthenia.
There is a partial bilateral harelip and a bilateral cleft palate. A shallow vertical groove marks the frontal bone between the tuberosities. The nasal bridge is flat, and the nasal bones vertical or absent. The rest of the nose is small, the alae being merely indicated, the nasolabial furrows ill-developed, and there is congenital occlusion of the nares. The central part of the upper lip, the prolabium, forms a narrow pyramidal projection whose base meets each half of the upper lip to form a notch. Between the notches, which are symmetrical, the apex of the prolabium is pendulous. There is possibly a congenital absence of the premaxillary element of the maxillary bones.
Presented (by) Herzfeld, GMA
The baby girl has curly reddish-brown hair, and her eyes are cast down; her right arm has been severed just below the elbow, the left arm just above. Her torso has been severed in the region of her diaphragm. She is indeed a ‘portion’: preserved, sometime in the mid-20th century, in a fluid-filled jar, to show a cleft palate and a malformation of the nose and jaw.
She died three weeks after she was born, of ‘asthenia’ – generalised weakness of the muscles.
The shape and positioning of her head and body bears a striking resemblance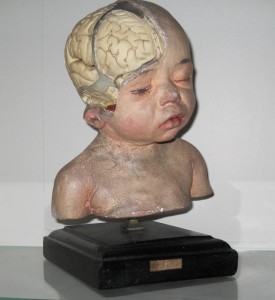 to another exhibit in the Museum, the plaster head of a baby, partly ‘dissected’ to show its brain.
to another exhibit in the Museum, the plaster head of a baby, partly ‘dissected’ to show its brain.
Was this deliberate?
Or, you might – as you become used to her features, when you have got past that ‘initial shock and recoil’ described by Joyce Gunn Cairns – see her as a work of art.
Frederik Ruysch (1638-1731), Dutch surgeon, anatomist and Konstenaar (artist), might have adorned her embalmed form with a necklace of blue-and-white beads, or small lace sleeves made by his daughter Rachel.
We can ask many questions: there is the ethical question of ‘parental consent’ about having one’s child used as a teaching specimen; the question whether creating such a specimen was justified for teaching/scientific purposes.
We can question why a half-torso is needed if the purpose is to show maldevelopment of the nasopharyngeal region.
We can also question why this preparation of a baby girl was donated by a female surgeon, the first female President of the RCSE, Gertrude Herzfeld.
Perhaps we could find some answers if we looked through the hospital’s and surgeon’s records, but that in itself would be unethical and in breach of patient privacy.
Let’s first of all consider Gertrude Herzfeld, (1890-1981): this is her Obituary from the British Medical Journal, volume 282, June 1981.
Miss Gertrude M A Herzfeld, who was formerly a consultant surgeon and a president of the Medical Women’s Federation, died on 12 May in her 91st year.
Gertrude Marianne Amalia Herzfeld was born at Hampstead, London, in 1890, and was educated at Edinburgh University, where she graduated in medicine in 1914. After house surgeon posts at the Royal Hospital for Sick Children and at Chalmers Hospital, Edinburgh, in 1917 she became a surgeon attached to the RAMC Cambridge Hospital, Aldershot, and from 1917 to 1919 was senior house surgeon at Bolton Infirmary.
After this she held many appointments as a consultant surgeon, being from 1920 to 1955 at Bruntsfield Hospital for Women and Children, and from 1920 to 1945 at the Royal Edinburgh Hospital for Sick Children. She was also surgeon to the Edinburgh Orthopaedic Clinic from 1925 to 1955 and a lecturer on the surgery of childhood at the university and a lecturer at the Edinburgh School of Chiropody.
Miss Herzfeld was chairman of the City of Edinburgh Division of the BMA from 1960 to 1962, a past president of the Medical Women’s Federation, president of the Soroptimist Club of Edinburgh in 1929, as well as more recent appointments such as vice-president of the Scottish Society of Women Artists since 1954, of the Edinburgh Cripple Aid Society since 1956, and of the Trefoil School for Physically Handicapped Children since 1964.
CVK writes: A remarkable woman has just died, full of years and memories for many generations of students. At the time of her birth her father went to business in a carriage. Gertrude always longed to be a doctor and this desire crystallised into surgery after a prizewinning career at Edinburgh University, which gave her an excellent training but retained its established hierarchical traditions. In the early days of the first world war a newly qualified woman with a German name did not find life easy; being the first woman to take a seat as a fellow in the Royal College of Surgeons of Edinburgh opened no ready gates.
Gertrude was a large woman in heart, mind, and build, and she saw fewer obstacles than others of her sex, because she knew what she had to do. At first her surgical patients were women only, but she soon established herself as an infinitely patient paediatric surgeon. None of her housemen could forget her great figure bending over a tiny neonate, opening and semi-constructing a blind cystic duct, easing a pyloric stenosis, or, later, apposing two raw edges of a minute cleft palate.
Her wards attracted patients with conditions that we had never seen as students. Before the days of chromosome determination, sex was mysteriously undefined in more children than we expected, and from all over Scotland they came for cosmetic repair and the difficult assessment of what course they were to follow.
This was done by a great deal more than surgery: infinite thought, getting to know the child, the mother, the surroundings – a psycho-somatic exercise in which Gertrude Herzfeld’s warmth and wisdom combined with her skill.
Students over half a century, undergraduate and postgraduate, will always remember the extra help and loyalty that Gertrude gave them; she never let us down in front of others, but quietly made it clear where we had erred; it was not a failure, but part of learning. She also taught the skill of loyalty to the general practitioner who sent us his patients. She understood.
***
Andrew Connell, Manager of Collections.
“On our first, superficial examination, all we saw was that the baby had a cleft palate. But we looked again, at the specimen, and at her notes – and saw that the girl had died at three weeks old, of ‘asthenia’, and that there were further complications in the nose and jaw region.
Let’s look at the possibilities:
What other incompatibilities, with life, does this condition bring? From Gertrude Herzfeld’s position, there is maybe nothing she can directly do (and the child is so malformed that she dies after three weeks).
Did Dr Herzfeld say explicitly that this specimen must go to the Royal College of Surgeons, did she emphasise this?
Was she even directly involved?
Maybe her name was just associated with the case. She may hardly even have seen it – the decision to preserve the baby was perhaps made somewhere else.
Herzfeld was a surgeon not a paediatric pathologist – she may not even have been to the post-mortem. She might have said, “I’d like someone to do a PM on this one, to find out what the internal organs are doing’: so the body goes off for autopsy.
In the Sick Kids hospital, the baby is taken to the PM room. And someone says, ‘This is quite unusual, let’s have it for the Museum.’
Then it comes here with the surgeon’s name on it.
Elsewhere the pathologist’s name might be on it, or on the histological slides in the records.
Since then (the baby could have died sometime in the period 1920-1950) there have been big changes in medical legislation and how records are kept. Records are now computerised, and there would be a field to complete for each person involved, surgeon, pathologist, histologist – all would be recorded, partly for litigation purposes. It would be easy to follow the ‘trail’.
Now, I’m just trying to think about why she should be here.
Is this demonstration of a cleft palate useful for teaching purposes? We missed the fact that the nasal bones hadn’t developed properly. Maybe that is why the specimen is here – is it unusual to have these two faults together? There aren’t any nostrils – what are the other implications for the respiratory tract?
Perhaps her preservation is also for posterity – the meaning might be ambiguous now, but in the future might give important clues.
So why the half-torso?
Why not the head, like ‘George’? To dissect that out takes time and skill.
What’s next easiest? To decapitate the body? But a detached head is probably more awkward, more offensive: it’s nastier.
What’s the next alternative? Dissect down to the shoulders – this too takes time and effort.
So why cut through at that plane, mid-torso, the arms as well?
The body could fit through a band-saw. This could have been the quickest method, chosen because it was the least unpleasant of the possibilities in order to present the specimen quickly.
Why not prepare the whole baby? It would be bulky and heavy. In an exam, a whole body might lead students to look for the wrong thing, in the wrong direction: ‘It’s got a boil on its bum’.”
On occasion, Andrew has had to change the fixative surrounding bottled specimens, including those of teratologically-deformed foetuses and neonates.
“Your eyes interpret things which aren’t true. A baby should be soft, it should be warm, babies are very tactile. But as specimens they are completely different. For example the weight, the fact that the body’s completely rigid, there’s no softness, no bending, no impression of your fingers on the skin. It’s slimy, almost like a fish, the texture is completely wrong. And they’re cold, very cold, almost like a rubber doll washed up on a beach. Something innate makes you feel the utmost respect. For example, if you need to put a needle through the ear, say, so as to fix the baby in position in the jar – it makes you cringe, it’s completely against nature, something unnatural.
I had to re-pot a dissected head that showed microcephaly – it was half external face, half internal dissection.
That was difficult because you can relate to a face, there’s the mouth, lips, teeth and all the rest.”
***
You can relate to a face: perhaps that’s why – once we have overcome our shock and intial revulsion – we can relate to ‘George’ and the cleft-palate baby.

